Current Science, and Conservative Care Strategies
Questions and Answers
Pelvic pain is a great challenge for men and women, and individuals can go for years before receiving a diagnosis. Pelvic pain can involve bladder pain, and other symptoms such as urinary urgency, frequency, hesitancy, incomplete emptying, urinary incontinence, and distress. Everybody is different! With bladder pain syndromes, there can be associated back, tailbone, hip or groin pain, bowel problems, and or pain with sexual function as well.
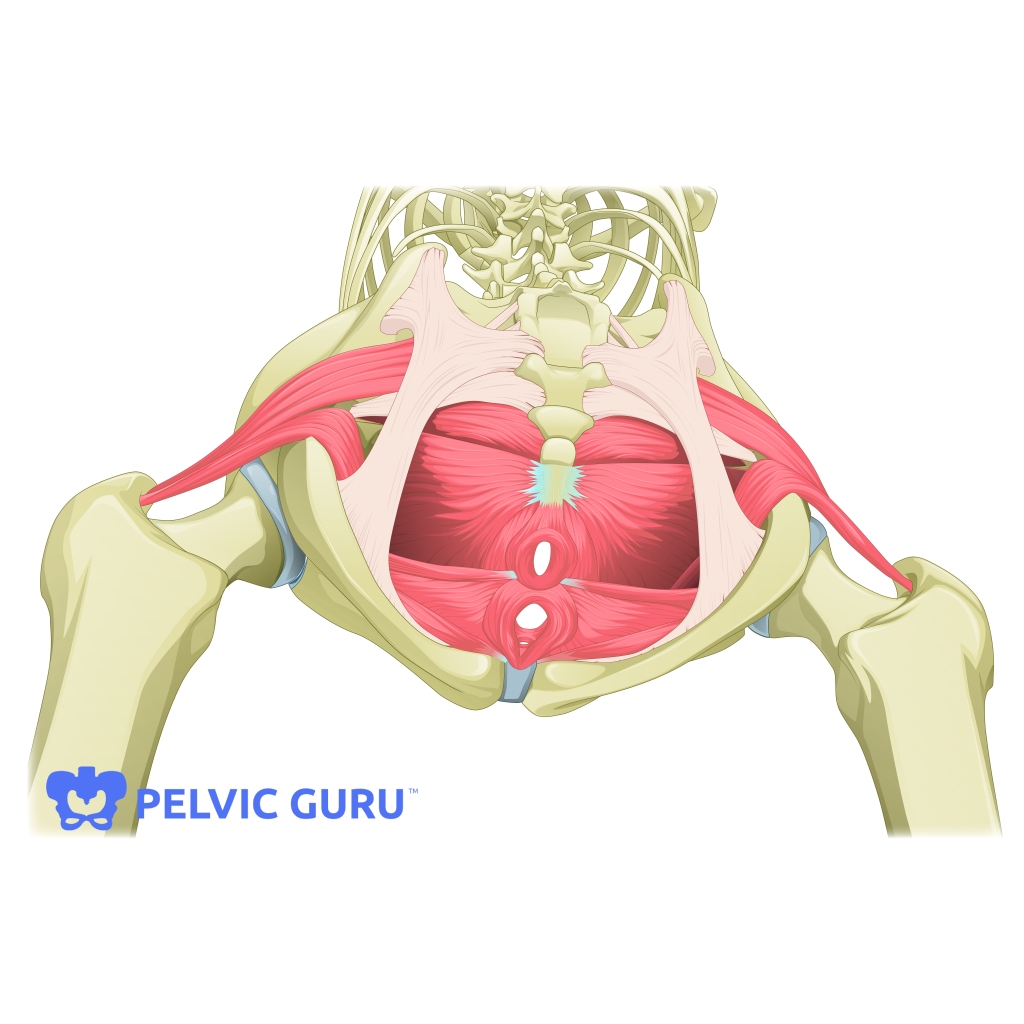
In Interstitial Cystitis (IC), sometimes there is an autoimmune component, with the walls of the bladder showing inflammation, which is viewed on a bladder scope (cystoscopy). In IC, the areas of inflammation are called Hunters Lesions. Or, sometimes women and men are diagnosed with bladder pain syndrome (BPS) based on symptoms. Always see your MD to assess the condition. Pelvic muscles surround the bladder, urethra and outlet into the penis or vagina. The bladder has 2 key jobs, 1.Storage.2.Emptying.

You may ask your doctor:
Is your Pain from Hunters lesions (HL IC) or Non Hunters lesions (N-HL IC/BPS)?
Irritation from a UTI or hunters lesion or other aggravating factor will often cause urinary urgency and frequency, that can persist over time. Those with the autoimmune type of IC may also have also have allergies, asthma, fibromyalgia, irritable bowel syndrome, thyroid disorders, ulcerative colitis, or other conditions, some of which can aggravate pelvic pain.
The goal of pelvic PT is to find out your pain provoking items, and put you in the driver’s seat for finding out your triggers and to develop optimum self -care.PT provides evaluation of all components of pain, and helps you discover if you have muscle spasm, shortening, weakness, lax or loose muscles, and helps you to train these muscles as needed. This may include biofeedback, home unit training for relaxation or strengthening, manual therapy/massage, behavioral habit training, bladder diaries, guides to nutrition resources and supplements as approved by the Interstitial cystitis association. Treatments may overlap for the two types of bladder pain problems, and include medical care with urologic testing, and medication, and possible instillations into the bladder.
Why PT for a bladder problem? Because we can address muscle based problems, as well as behavioral training and guide you to nutrition resources.
Conservative Care: PT: What we do: The goal of PT is to reduce and or eliminate your symptoms with conservative care. This involves detective work. Also, PT often uses mind body practices and exercise, such as yoga and meditation for pelvic pain.
A key research study found PT using myofascial therapy helped with significant pain reduction in individuals with IC/BPS (see Fitzgerald et al). 87% of patients with IC/BPS have tender or trigger points in muscles, and there was 59% improved in Pelvic Floor PT, and 26% with general massage! PT and massage therapy are a great combination.
Experts agree: “The vast majority of patients with N-HL IC/BPS need management of their pelvic floor muscles as the primary therapy, complemented by bladder-directed therapies as needed as well as a multidisciplinary team to manage a variety of other regional/systemic symptoms.” (direct quote Han et al).
You may wonder how and why you developed IC/BPS, and according to research, Chronic Pelvic Pain may be linked to a number of factors, such as :
Birth history (your own history of cesarean vs vaginal birth)
Genetics making you susceptible to autoimmune illness
Environmental influences, (Gut biome, nutrition, and your health history such as UTI, Surgeries, childbirth, exposure to yeast, mold, parasites, or bacteria).
Psychosocial profile: mood, traits, and sleep quality
Adverse Childhood Experiences (ACE)
So with all of this information in mind, consider that there are many elements to improving health and wellness, and many people reduce their bladder symptoms by shifting habits, nutrition, and so forth; consider resiliency and that the bladder can improve with the right combination of treatments over time.
Is your gut involved?
Recent research is looking into the gut biome, which is the network of probiotic and prebiotic organisms in the digestive tract that help us rest, digest, support immunity, create vitamins and nerve transmitters…and found:
“IC/BPS is associated with significant morbidity, yet underlying mechanisms and diagnostic biomarkers remain unknown. Pelvic organs exhibit neural crosstalk by convergence of visceral sensory pathways, and rodent studies demonstrate distinct bacterial pain phenotypes, suggesting that the microbiome modulates pelvic pain in IC. Stool samples were obtained from female IC patients and healthy controls, and symptom severity was determined by questionnaire.” Testing “demonstrated significantly reduced levels of E. sinensis, C. aerofaciens, F. prausnitzii, O. splanchnicus, and L. longoviformis in microbiota of IC patients. These species, deficient in IC pelvic pain (DIPP), were further evaluated, and “DIPP species emerged as potential IC biomarkers.” (Braundmeier-Fleming et al).
There is a bladder biome as well, and research is expanding on this topic over time. If your biome is lacking in helpful species, or has an overgrowth of certain bacteria, most patients are left to trial and error in the use of probiotics, as we do not yet have big studies on IC/BPS. You can ask your health care provider if they have a brand they recommend, and patients should start on the lowest dose and note any symptoms positive or negative. Hopefully future studies will clarify the topic.
Attendees at the San Diego IC support group have shared success stories over the years, with strategies that were individualized, and you can connect with others for healthcare support via this link:
For more information on IC/BPS please consult the ichelp.org website and you will find I care videos, which is the Interstitial Cystitis Awareness Research and Education component developed for those suffering; icarevideos; This includes 15 videos with topics ranging from pain management, strategies for sexual activities, mindfulness, nutrition to dial down inflammation, diagnostic testing, male prostatitis vs IC, and other topics.
http://www.ichelp.org/icarevideos
Check out other mypelvicrehab.wordpress.com blogs to learn more, including anatomy information, this (pelvic problems, pain, IC, Pelvic PT) is all generally a topic not discussed much and facts and resources for care are expanding over time.
Function Smart PT 10803 Vista Sorrento Parkway, San Diego CA 92121, 858 452 0282
Maureen Mason DPT, WCS, PYT. Maureen@functionsmart.com mypelvicrehab.wordpress.com
References:
Bedaiwy MA, Patterson B and Mahajan S. Prevalence of myofascial chronic pelvic pain and the effectiveness of pelvic floor physical therapy. J Reprod Med 2013; 58: 504–510.
Braundmeier-Fleming A, Russel N T, Wenbin Y, et al. Stool-based biomarkers of interstitial cystitis/bladder pain syndrome, Scientific Reports 2016
Cozean N, Pelvic floor physical therapy in the treatment of a patient with interstitial cystitis, dyspareunia, and low back pain, J Women’s Health PT 2017, 41(1)
Fitzgerald MP, Anderson RU, Potts J, et al. Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J Urol 2009; 182: 570–580.
Han E, Nguyen L, Sirls L, Peterson K, Current best practice in management of interstitial cystitis/bladder pain syndrome, Therapeutic Advances in Urology 2018,10(7) 197-211
Peters KM, Carrico DJ, Kalinowski SE, et al. Prevalence of pelvic floor dysfunction in patients with interstitial cystitis. Urology 2007; 70: 16–18. 82.
Russell N, Daniels B, Smoot B, et al; Effects of yoga on quality of life and pain in women with chronic pelvic pain: Systematic review and meta-analysis, J Women’s Health Physical Therapy 2019, 43(3);144-154
Weiss JM. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J Urol 2001; 166: 2226–2231. 83.

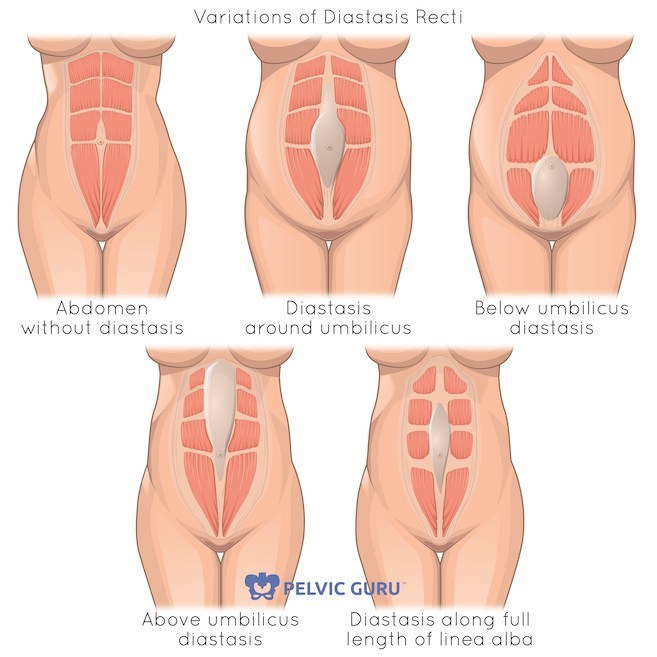




 Be an advocate for yourself and speak to your health care provider to obtain a prescription for specialty Pelvic PT, with goals to increase your comfort, confidence, safety, and fitness power during the pregnancy and in preparation for baby care. Direct access also allows women to come in independently for musculoskeletal screening, such as diastasis rectus abdominus testing, load transfer and body mechanics, sacro -iliac and pubic symphysis alignment, pain and spasm, and biomechanic analysis. (Also I screen for red flags such as high blood pressure which may sneak up on you). Pelvic muscles and the abdomen and spine can benefit from mini workouts and longer exercise routines as needed. Women who exercise at their own comfort level and capacity have better pregnancy outcomes in general re shorter labors and interventions.Also, binders, belts and belly bands may help and we can offer expert advice and equipment sampling.
Be an advocate for yourself and speak to your health care provider to obtain a prescription for specialty Pelvic PT, with goals to increase your comfort, confidence, safety, and fitness power during the pregnancy and in preparation for baby care. Direct access also allows women to come in independently for musculoskeletal screening, such as diastasis rectus abdominus testing, load transfer and body mechanics, sacro -iliac and pubic symphysis alignment, pain and spasm, and biomechanic analysis. (Also I screen for red flags such as high blood pressure which may sneak up on you). Pelvic muscles and the abdomen and spine can benefit from mini workouts and longer exercise routines as needed. Women who exercise at their own comfort level and capacity have better pregnancy outcomes in general re shorter labors and interventions.Also, binders, belts and belly bands may help and we can offer expert advice and equipment sampling.


